MedPage Today Article Rating
MedPage Today Article RatingBiden Proposes Coverage of Obesity Drugs in Medicare, Medicaid
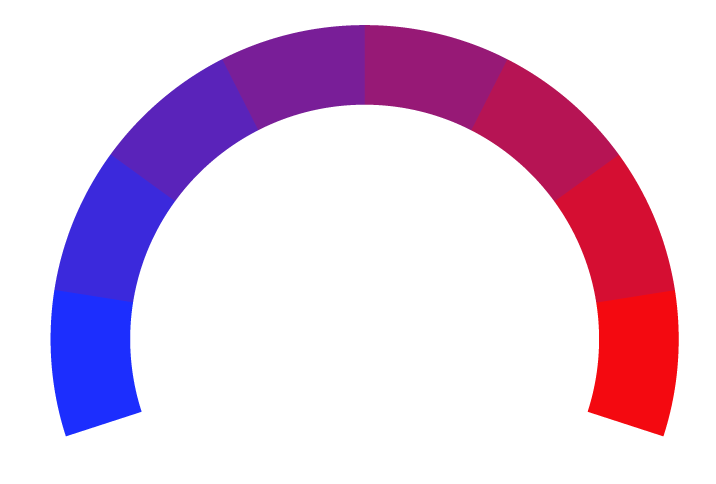
- Bias Rating
12% Somewhat Conservative
- Reliability
70% ReliableGood
- Policy Leaning
12% Somewhat Conservative
- Politician Portrayal
N/A
Continue For Free
Create your free account to see the in-depth bias analytics and more.
Continue
Continue
By creating an account, you agree to our Terms and Privacy Policy, and subscribe to email updates. Already a member: Log inBias Score Analysis
The A.I. bias rating includes policy and politician portrayal leanings based on the author’s tone found in the article using machine learning. Bias scores are on a scale of -100% to 100% with higher negative scores being more liberal and higher positive scores being more conservative, and 0% being neutral.
Sentiments
2% Positive
- Liberal
- Conservative
| Sentence | Sentiment | Bias |
|---|---|---|
Unlock this feature by upgrading to the Pro plan. | ||
Reliability Score Analysis
Policy Leaning Analysis
Politician Portrayal Analysis
Bias Meter
Extremely
Liberal
Very
Liberal
Moderately
Liberal
Somewhat Liberal
Center
Somewhat Conservative
Moderately
Conservative
Very
Conservative
Extremely
Conservative
-100%
Liberal
100%
Conservative
Contributing sentiments towards policy:
54% : Medicare and Medicaid recipients with obesity would have access to coverage of pricey GLP-1 receptor agonists like semaglutide (Wegovy) or tirzepatide (Zepbound) under a regulation proposed Tuesday by the Centers for Medicare & Medicaid Services (CMS).51% : This is similar to what the agency did when it came to covering drugs to combat wasting and cachexia in AIDS patients, Meena Seshamani, MD, PhD, director of the Center for Medicare, said on the call.
51% : "As for the cost of coverage, CMS estimates that Medicare will spend $25 billion over a 10-year period on the GLP-1 drug coverage, Seshamani said.
50% : On the Medicaid side, CMS estimates that the cost will be $14.8 billion over 10 years, with the federal government picking up $11 billion and the states paying the remainder, Dan Tsai, director of the Center for Medicaid and CHIP, said on the call.
47% : "States are feeling substantial state budget pressure, and we are doing our part to make sure that patients, Medicaid enrollees all across the country can get access to life-saving and life-altering medications," he said.
42% : Historically, this has meant that drugs used for weight loss, even when used for treatment of individuals with obesity, have been excluded from Medicare prescription drug coverage for Medicaid," with some states covering them and others not.
*Our bias meter rating uses data science including sentiment analysis, machine learning and our proprietary algorithm for determining biases in news articles. Bias scores are on a scale of -100% to 100% with higher negative scores being more liberal and higher positive scores being more conservative, and 0% being neutral. The rating is an independent analysis and is not affiliated nor sponsored by the news source or any other organization.